Many public health bodies are responding to crisis by shifting their attention and resources from (1) a long-term strategic focus on reducing non-communicable diseases (such as heart diseases, cancers, diabetes), to (2) the coronavirus pandemic.
Of course, these two activities are not mutually exclusive, and smoking provides the most high-profile example of short-term and long-term warnings coming together (see Public Health England’s statement that ‘Emerging evidence from China shows smokers with COVID-19 are 14 times more likely to develop severe respiratory disease’).
There are equally important lessons – such as on health equity – from the experiences of longer-term and lower-profile ‘preventive’ public health agendas such as ‘Health in All Policies’ (HIAP).*
What is ‘Health in All Policies’?
HIAP is a broad (and often imprecise) term to describe:
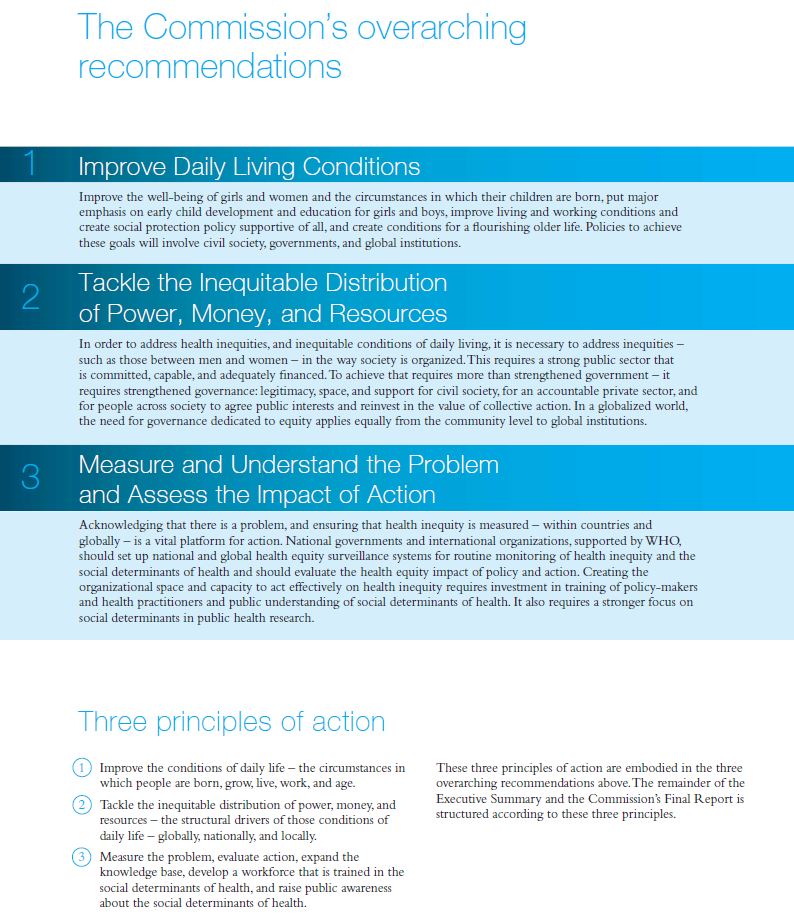
- The policy problem. Address the ‘social determinants’ of health, defined by the WHO as ‘the unfair and avoidable differences in health status … shaped by the distribution of money, power and resources [and] the conditions in which people are born, grow, live, work and age’.
- The policy solutions. Identify a range of policy instruments, including redistributive measures to reduce economic inequalities, distributive measures to improve public services and the physical environment (including housing), regulations on commercial and individual behaviour, and health promotion via education and learning.
- The policy style. An approach to policymaking that encourages meaningful collaboration across multiple levels and types of government, and between governmental and non-governmental actors (partly because most policy solutions to improve health are not in the gift of health departments).
- Political commitment and will. High level political support is crucial to the production of a holistic strategy document, and to dedicate resources to its delivery, partly via specialist organisations and the means to monitor and evaluate progress.
As two distinctive ‘Marmot reviews’ demonstrate, this problem (and potential solutions) can be described differently in relation to:
Either way, each of the 4 HIAP elements highlights issues that intersect with the impact of the coronavirus: COVID-19 has a profoundly unequal impact on populations; there will be a complex mix of policy instruments to address it, and many responses will not be by health departments; an effective response requires intersectoral government action and high stakeholder and citizen ownership; and, we should not expect current high levels of public, media, and policymaker attention and commitment to continue indefinitely or help foster health equity (indeed, even well-meaning policy responses may exacerbate health inequalities).
A commitment to health equity, or the reduction of health inequalities
At the heart of HIAP is a commitment to health equity and to reduce health inequalities. In that context, the coronavirus provides a stark example of the impact of health inequalities, since (a) people with underlying health conditions are the most vulnerable to major illness and death, and (b) the spread of underlying health conditions is unequal in relation to factors such as income and race or ethnicity. Further, there are major inequalities in relation to exposure to physical and economic risks.
A focus on the social determinants of health inequalities
A ‘social determinants’ focus helps us to place individual behaviour in a wider systemic context. It is tempting to relate health inequalities primarily to ‘lifestyles’ and individual choices, in relation to healthy eating, exercise, and the avoidance of smoking and alcohol. However, the most profound impacts on population health can come from (a) environments largely outside of an individual’s control (e.g. in relation to threats from others, such as pollution or violence), (b) levels of education and employment, and (c) economic inequality, influencing access to warm and safe housing, high quality water and nutrition, choices on transport, and access to safe and healthy environments.
In that context, the coronavirus provides stark examples of major inequalities in relation to self-isolation and social distancing: some people have access to food, private spaces to self-isolate, and open places to exercise away from others; many people have insufficient access to food, no private space, and few places to go outside (also note the disparity in resources between countries).
The pursuit of intersectoral action
A key aspect of HIAP is to identify the ways in which non-health sectors contribute to health. Classic examples include a focus on the sectors that influence early access to high quality education, improving housing and local environments, reducing vulnerability to crime, and reforming the built environment to foster sustainable public transport and access to healthy air, water, and food.
The response to the coronavirus also appears to be a good advert for the potential for intersectoral governmental action, demonstrating that measures with profound impacts on health and wellbeing are made in non-health sectors, including: treasury departments subsidising business and wages, and funding additional healthcare; transport departments regulating international and domestic travel; social care departments responsible for looking after vulnerable people outside of healthcare settings; and, police forces regulating social behaviour.
However, most (relevant) HIAP studies identify a general lack of effective intersectoral government action, related largely to a tendency towards ‘siloed’ policymaking within each department, exacerbated by ‘turf wars’ between departments (even if they notionally share the same aims) and a tendency for health departments to be low status, particularly in relation to economic departments (also note the frequently used term ‘health imperialism’ to describe scepticism about public health in other sectors). Some studies highlight the potential benefits of ‘win-win’ strategies to persuade non-health sectors that collaboration on health equity also helps deliver their core business (e.g. Molnar et al 2015), but the wider public administration literature is more likely to identify a history of unsuccessful initiatives with a cumulative demoralising effect (e.g. Carey and Crammond, 2015; Molenveld et al, 2020).
The pursuit of wider collaboration
HIAP ambitions extend to ‘collaborative’ or ‘co-produced’ forms of governance, in which citizens and stakeholders work with policymakers in health and non-health sectors to define the problem of health inequalities and inform potential solutions. These methods can help policymakers make sense of broad HIAP aims through the eyes of citizens, produce priorities that were not anticipated in a desktop exercise, help non-health sector workers understand their role in reducing health inequalities, and help reinforce the importance of collaborative and respectful ways of working.
An excellent example comes from Corburn et al’s (2014) study of Richmond, California’s statutory measures to encourage HIAP. They describe ‘coproducing health equity in all policies’ with initial reference to WHO definitions, but then to social justice in relation to income and wealth, which differs markedly according to race and immigration status. It then reports on a series of community discussions to identify key obstacles to health:
“For example, Richmond residents regularly described how, in the same day, they might experience or fear violence, environmental pollution, being evicted from housing, not being able to pay health care bills, discrimination at work or in school, challenges accessing public services, and immigration and customs enforcement (ICE) intimidation … Also emerging from the workshops and health equity discussions was that one of the underlying causes of the multiple stressors experienced in Richmond was structural racism. By structural racism we meant that seemingly neutral policies and practices can function in racist ways by disempowering communities of color and perpetuating unequal historic conditions” (2014: 627-8).
Yet, a tiny proportion of HIAP studies identify this level of collaboration and new knowledge feeding into policy agendas to address health equity.
The cautionary tale: HIAP does not cause health equity
Rather, most of the peer-reviewed academic HIAP literature identifies a major gap between high expectations and low implementation. Most studies identify an urgent and strong impetus for policy action to be proportionate to the size of the policy problem, and ideas about the potential implementation of a HIAP agenda when agreed, but no studies identify implementation success in relation to health equity. In fact, the two most-discussed examples – in Finland and South Australia – seem to describe a successful reform of processes that have a negligible impact on equity.
A window of opportunity for what?
It is common in the public health field to try to identify ‘windows of opportunity’ to adopt (a) HIAP in principle, and (b) specific HIAP-friendly policy instruments. It is also common to try to identify the factors that would aid HIAP implementation, and to assume that this success would have a major impact on the social determinants of health inequalities. Yet, the cumulative experience from HIAP studies is that governments can pursue health promotion and intersectoral action without reducing health inequalities.
For me, this is the context for current studies of the unequal impact of the coronavirus across the globe and within each country. In some cases, there are occasionally promising discussions of major policymaking reforms, or to use the current crisis as an impetus for social justice as well as crisis response. Yet, the history of the pursuit of HIAP-style reforms should help us reject the simple notion that some people saying the right things will make that happen. Instead, right now, it seems more likely that – in the absence of significantly new action** – the same people and systems that cause inequalities will undermine attempts to reduce them. In other words, health equity will not happen simply because it seems like the right thing to do. Rather, it is a highly contested concept, and many people will use their power to make sure that it does not happen, even if they claim otherwise.